Insulin Secretion - The Untold Story
It is a well known fact that Insulin is secreted from the beta cells of the pancreas.
But how much more do we really know about the secretion of this hormone that governs so many of our metabolic pathways?
Let us try to fully understand the process by which this peptide hormone finds its way into our blood.
First things first, what is insulin and how is it made?
The gene that codes for insulin is called the insulin gene or the INS gene and it is located on Chromosome 11p15. When this gene is translated, it makes a 110 amino acid polypeptide called pre-pro-insulin. While it is transported from the endoplasmic reticulum to the Golgi apparatus, a signal polypeptide is cleaved off, leaving only pro-insulin. Pro-insulin enters the golgi apparatus and is packed into a neat secretory vesicle. Once inside this vesicle, pro-insulin is cleaved to give insulin and C-peptide. These are both stored in the vesicle and are released together when the depolarization of the beta cell occurs.
Now that insulin is made and it is stored, how and when does it come out of the beta cells?
Before we dive into the secretion of insulin proper, there are two things that we must know about the basal state of the beta cells of the pancreas.
- Insulin, after synthesis, is stored in vesicles within the beta cell.
- The beta cell is in a constant state of hyperpolarization.
Hyperpolarization? Why does that matter, you might ask. You see, most cells in our body stay in a state of equilibrium and maintain their resting membrane potential. However the beta cells of the pancreas are always hyperpolarized because of a constantly functioning ATP dependant potassium ion channel that is present on the cell membrane. This channel causes a constant loss of potassium from the cell. As a result, there is a constant loss of (+) charge from the cell which keeps the cell hyperpolarized.
Now, in our body, in order for any substance stored in a vesicle to come out into the extracellular fluid, Calcium entry into the cell is required. And, in order for calcium to enter the cell, the cell must first reach a depolarised state. But since the beta cells are constantly in a hyperpolarized state due to the potassium leak, this calcium entry doesn’t happen and the insulin stored in the vesicles stays there.
Well we got to get the insulin out right? So here's how the body goes about depolarizing the beta cell.
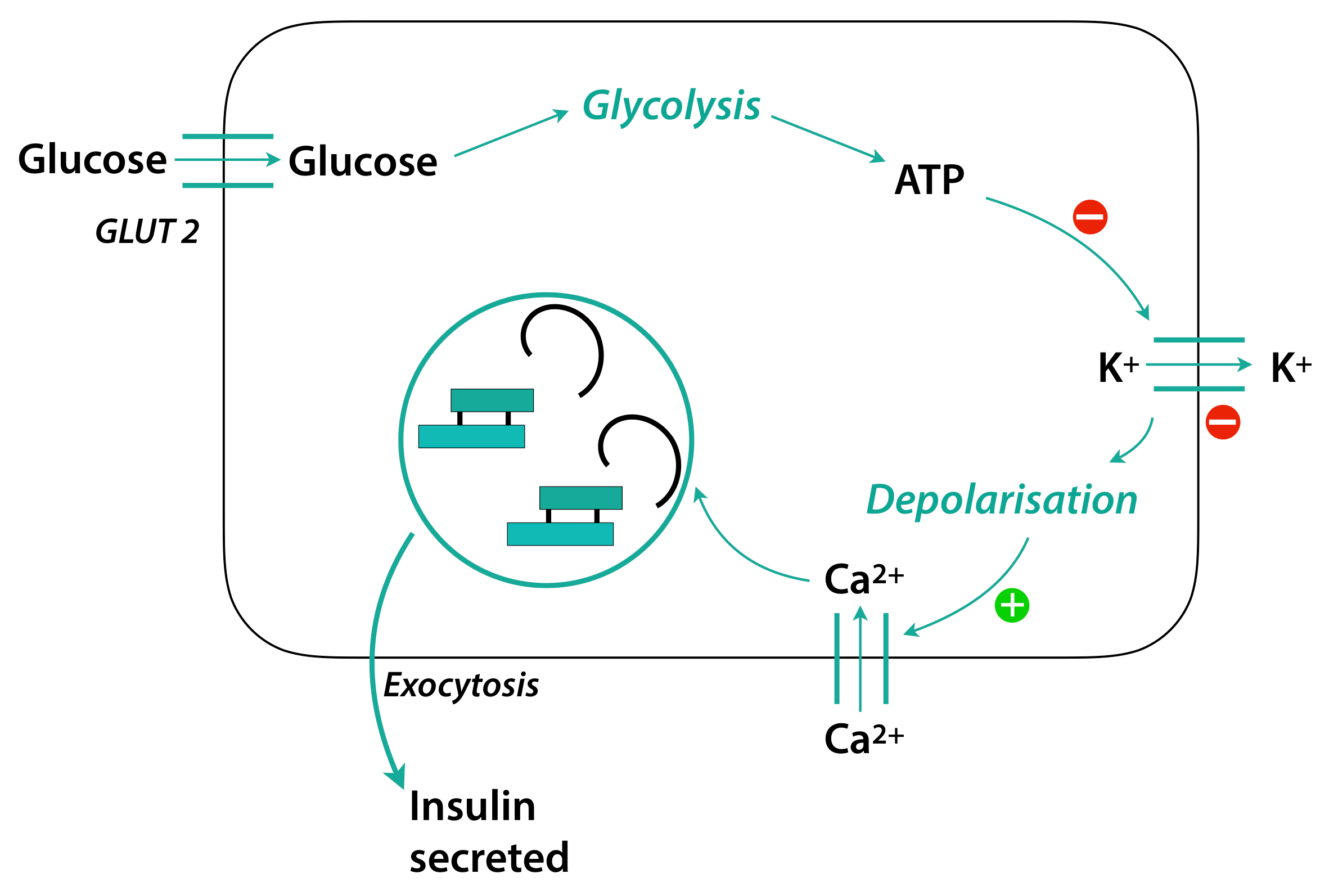
The process begins with the ingestion of food. The secretion of insulin can be stimulated by many substances like fatty acids and amino acids but the most potent stimulus for insulin release is glucose. So once food is ingested and broken down into its constituent parts, the glucose enters the beta cells of the pancreas through the GLUT - 2 transporter.
The GLUT 2 transporter, you must remember, is independent of insulin. This means that it is always present on the cell surface and it is always working.
Once inside the cell, the glucose undergoes glycolysis, which is the process of breaking down glucose to form ATP. Once the ATP is formed, it acts on the ATP dependent potassium ion channel and inhibits it.
This results in inhibition of the potassium leak and once this happens, the cell slowly goes from being hyperpolarized to being depolarized.
As soon as a threshold potential is reached, the voltage gated Calcium channels open up and calcium floods into the cell. This causes the vesicles of insulin to merge with the cell membrane and the insulin is released into the blood by exocytosis.
This information about the workings of the beta cell and the physiology of insulin secretion helps us tremendously when treating conditions of the pancreas. You see, the potassium channel that causes the constant leak of potassium and kept the cell hyperpolarized is manipulated to increase or decrease insulin production.
If that channel is inhibited then it will cause more insulin to be released. This property is used in treating Diabetes Mellitus, where more insulin is needed to keep high glucose levels in check. Potassium channel inhibitors like sulphonylureas and meglitinides are used to achieve this.
If that channel is opened up or stimulated, then very little insulin will be secreted. This is property is used to treat a condition called insulinoma. An insulinoma is a tumour of the beta cells of the pancreas which secretes excessive amounts of insulin. Potassium channel openers like diazoxide may be used.
Understanding insulin and its secretion is a stepping stone into the world of hormones. Endocrine physiology – the “why” behind the functioning of our body is a stunningly elaborate field which hides many intricate pathways. These pathways and interactions between little molecules and our complex body, one could argue, is what makes us humans. But, only a few of these have been fully understood and elucidated and the rest may well hold the key to a better, brighter and healthier future.
Author: Narendran Sairam (Facebook)
Sources and citations
“INS Gene - Genetics Home Reference.” U.S. National Library of Medicine, National Institutes of Health, 19 Dec. 2017, ghr.nlm.nih.gov/gene/INS.
Fu, Zhuo, et al. “Regulation of Insulin Synthesis and Secretion and Pancreatic Beta-Cell Dysfunction in Diabetes.” Current Diabetes Reviews, U.S. National Library of Medicine, 1 Jan. 2013, www.ncbi.nlm.nih.gov/pmc/articles/PMC3934755/.