Pterygium - A Winged Menace
What is it?
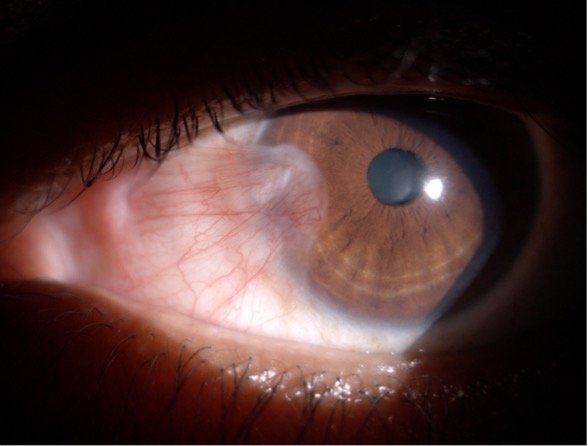
It is a fibrovascular, wing-shaped encroachment of the conjunctiva onto the cornea.
Risk Factors
Excessive UV exposure
Microtrauma
Chronic inflammation from environmental factors
Pathogenesis
UV rays cause the insufficiency of the limbal stem cells of the cornea.
It causes activation of the tissue growth factors, which further lead to angiogenesis and cell proliferation.
The limbal stem cells are damaged by the UV rays that cause conjunctivalization of the cornea, and the cornea is invaded by aggressive fibroblasts.
UV radiation may cause mutations in the p53 tumor suppressor gene, resulting in the abnormal pterygial epithelium.
Occurring in two stages: the initial disruption of the limbal corneal-conjunctival epithelial barrier, and the progressive “conjunctivalization” of the cornea characterized by cellular proliferation, inflammation, connective tissue remodeling, and angiogenesis
Human papillomavirus could also be involved in the pathogenesis of the pterygium.
Pathology
Accumulation of degenerated subepithelial tissue which is basophilic with a characteristic slate gray appearance on H&E staining.
Vermiform or elastotic degeneration.
Destruction of Bowman layer by fibrovascular ingrowth is typical.
The overlying epithelium is usually normal, but may be acanthotic, hyperkeratotic, or even dysplastic and often exhibits areas of goblet cell hyperplasia.
Parts of a Pterygium
Cap
A semilunar infiltrating portion in front of the head showing opaque spots (Fuch’s spots) suggestive of progression
Head
Invading portion which contains the apex of the tissue is called the head
Neck
Area between head and body.
Body
Remaining bulk of mass connecting with the bulbar conjunctiva.
Image: Rajan Eye Care Hospital.
Types of Pterygium
Progressive pterygium
Thick, fleshy, vascular, progressively encroaching towards the center of the cornea.
Atrophic Pterygium
Thin, attenuated, poor vascularity, stationary.
Symptoms
Redness
Irritation
Watering
Foreign body sensation
Reduced vision - if the pupillary axis is involved.
What to look for in examination?
1.Location
Whether nasal or temporal. Pterygiums are most commonly nasal.
2. Progression
Progressive pterygium are fleshy and have increased vascularity.
3. Extent
If they are encroaching onto the cornea and if they involve the pupillary axis.
4. Fuch’s Flecks
Subepithelial deposits ahead of the head of pterygium suggestive of progression.
5.Stocker’s line
Iron pigmentation line suggestive of the chronicity of the pterygium.
6. Restriction of movement
Might be present if the pterygium is recurrent.
7. Inflammation
8. Keratometry
9.Disc status
Differential Diagnosis of Pterygium
Corneal phlyctenule.
Elevated pinguecula.
Limbal dermoid.
Ocular surface squamous neoplasia (OSSN).
Papilloma.
Nodular scleritis.
Grading Systems
Tan et al
T1: Atrophic pterygia: pterygia with visible episcleral vessels beneath the body
T2: Intermediate Pterygia: Partially obscured episcleral vessels.
T3: Fleshy pterygium with all episcleral vessels obscured by the opaque fibrovascular tissue of the pterygium body.
Grading the effect of Pterygium on Corneal Topography
Grade 1: pterygium whose head is located between limbus and a point midway between limbus and pupil.
Grade 2: indicates the pterygium with the head located between a point midway between limbus and pupillary margin and pupillary margin.
Grade 3: the head crosses the pupil margin.
Grading of recurrent Pterygium
Grading is based on external appearance.
Grade 1: cases with a normal operative site.
Grade 2: presence of fine episcleral vessels without fibrous tissue.
Grade 3: cases with fibrous tissue not invading the cornea.
Grade 4: true recurrent pterygia with a fibrovascular tissue invading the cornea
Johnston Grading System
This was the first comprehensive grading system used for Pterygium in clinical research.
The main components of these grading systems included hyperemia, translucency, and the vascular network of the pterygium which are determined by images take in the primary and lateral gaze. The hyperemia of both head and body are considered for this.
Grade 0: no pterygium tissue presents.
Grade 1: consists of an indistinguishable translucent tissue with visible underlying episcleral vessels.
The main feature of pterygium in this grade is dilated vessels, compared with the normal surrounding conjunctival vessels.
Grade 2: pink tissue with increased density of vessels.
The pterygium is translucent enough to allow the examiner to distinguish episcleral vessels.
Grader 3: the pterygium is red in colour, the vessels are engorged and tortuous, and the underlying episcleral vessels are indistinguishable.
Grade 4: Severe pterygium: deep and diffusely red tissue that completely obscures the underlying scleral tissue.
Complications of Pterygium
Corneal astigmatism: causes with-the-rule astigmatism due to the flattening of the horizontal meridian along its leading head. [8]
The formation of a tear meniscus between the corneal center and the pterygium apex has been proposed for the underlying mechanism of horizontal corneal flattening.
Management of Pterygium
Indications of surgery
Pterygium encroaching upon the pupillary area causing dimunition of vision.
Distortion of vision due to high astigmatism.
Recurrent inflammation.
Limited eye movement.
Cosmetic reasons.
Surgical Options
Bare Sclera Technique
·The isolated bare sclera technique is the quickest surgical approach to pterygium removal, requiring the least tissue manipulation.
High postoperative recurrence rate of pterygium.
Adjuvant MMC with bare sclera technique can reduce the recurrence rate.
Conjunctival / Conjunctival Limbal Autograft
Covering the scleral bed with a free graft harvested from adjacent conjunctiva (usually superior) after pterygium removal.
Lower recurrence rates.
The graft can be fixated to the adjacent tissue by vicryl sutures or fibrin glue.
Amniotic Membrane Transplant
Stromal component and overlying basal lamina of AM resemble the architecture of normal human conjunctiva, where it can provide a platform for the growth of conjunctival and corneal epithelial layer.
The covering feature of AM reduces postoperative pain through protecting scleral nerve ends and reduces evaporation
Complications of Pterygium Surgery
Intraoperative
Excessive bleeding (Can be reduced by a drop of brimonidine/ phenylephrine prior to surgery as they are vasoconstrictors).
Postoperative
Graft edema.
Inversion of the graft.
Hematoma under the graft.
Corneal scarring.
Scleral thinning/ ulceration (with use of beta radiation/ MMC).
Author: Madhuvanthi Mohan
Sources and citations
1) Di Girolamo N, Chui J, Coroneo MT, Wakefield D. Pathogenesis of pterygia: role of cytokines, growth factors, and matrix metalloproteinases. Prog Retin Eye Res. 2004 Mar;23(2):195-228.
2) Hamed-Azzam S, Edison N, Briscoe D, Mukari A, Elmalah I. Identification of human papillomavirus in pterygium. Acta Ophthalmol. 2016 May.
3) Reid TW, Dushku N. Does human papillomavirus cause pterygium? Br J Ophthalmol. 2003 Jul;87(7):806-8.
4) (Tan DT, Chee SP, Dear KB, et al. Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol 1997; 115: 1235–1240)
5) Maheshwari S. Pterygium-induced corneal refractive changes. Indian J Ophthalmol 2007; 55: 383–386
6) (Prabhasawat P, Barton K, Burkett G, et al. Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology 1997; 104: 974–985.)
7) (Johnston SC, Williams PB, Sheppard JD., Jr.A comprehensive system for pterygium classification. Invest Ophthalmol Vis Sci 2004; 45: 2940. )
8) (Tomidokoro A, Miyata K, Sakaguchi Y, et al. Effects of pterygium on corneal spherical power and astigmatism.)